
The newly-appointed Prince Philip Professor of Technology discusses a fast-growing field.
Could brain interfaces enable us to treat a wide range of diseases?
In the 1780s, Italian physician Luigi Galvani discovered that he could make a dead frog’s legs twitch when he applied an electrical spark to the sciatic nerve.
With these experiments, the field of bioelectricity was born.
It took until 1958 for the first medical device using the phenomenon to be inserted into the body, when a pacemaker was implanted into a patient at Karolinska Hospital.
Today, pacemakers remain by far the most common implantation device, followed by cochlea implants to treat hearing impairments.
There are others: stimulators for the spinal cord to alleviate pain, for example, and deep brain stimulators for treating the tremors or shuffling gait associated with Parkinson’s disease.
The potential for bioelectronics is much wider, however. Implants that deliver electrical signals to our nerves could one day be used to treat all manner of conditions, from asthma to diabetes, arthritis to chronic obstructive pulmonary disease.
They might eventually replace many of today’s drugs, eliminating side effects and overcoming issues of toxicity in one fell swoop.
Professor George Malliaras, who has been appointed the Prince Philip Professor of Technology at Cambridge, named after the university’s former chancellor, is busy setting up his lab at the Nanoscience Centre to continue his work on using bioelectronics and organic electronics to create novel implantable devices that interface with the brain.
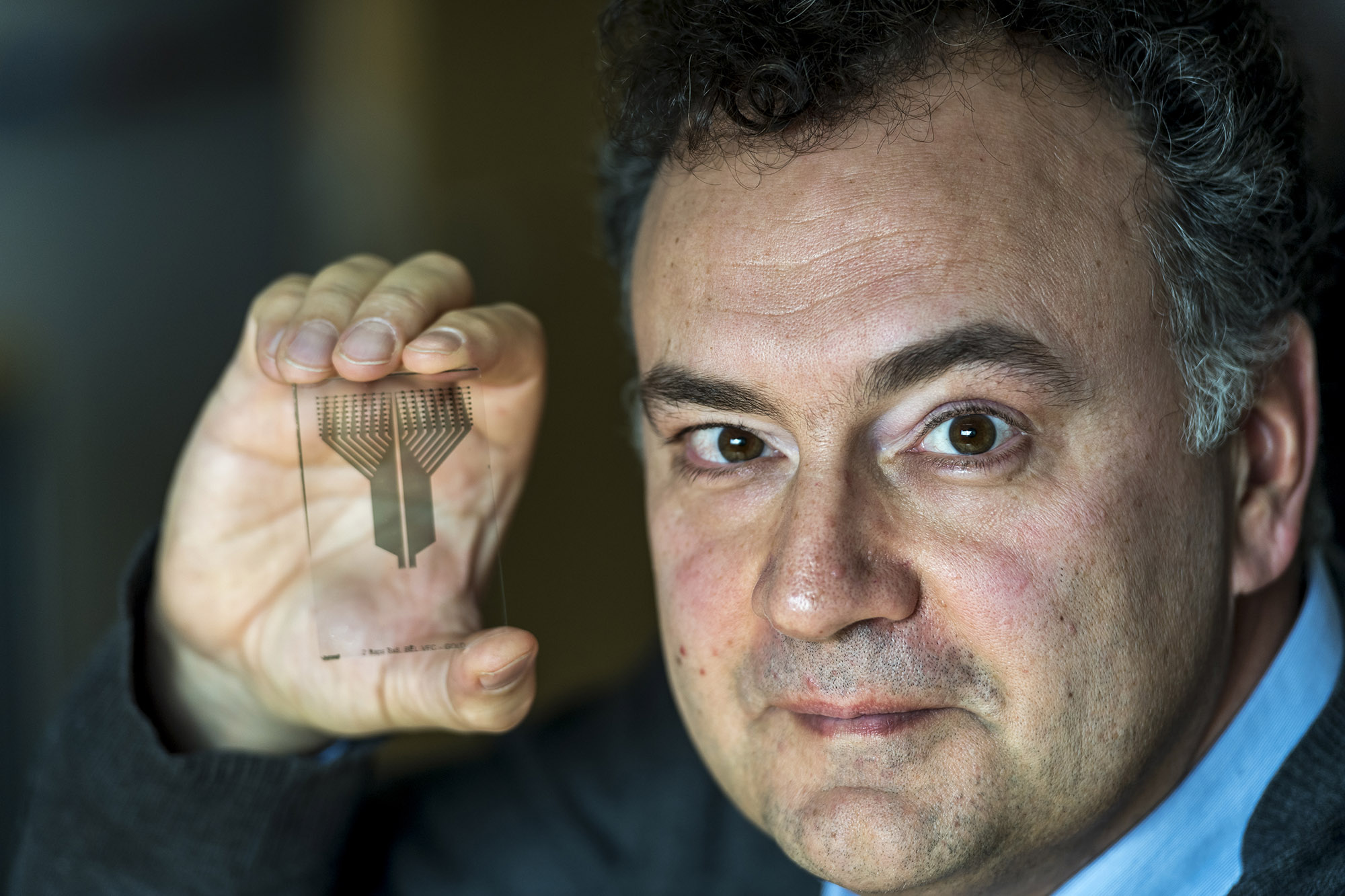
George Malliaras with one of his recording devices. Picture: Keith Heppell
Among those who could benefit are patients with epilepsy, for whom standard treatments are not successful or suitable.
“Epilepsy is an umbrella term covering many conditions associated with seizures,” says Professor Malliaras, who is connected to the Department of Engineering.
“Usually it is treated by anti-convulsant drugs that were first developed in the 1950s and about 30 per cent of patients were drug resistant. Today, that hasn’t changed. The drugs have improved significantly – they have fewer side effects and require less frequent administration, but there is a very stubborn 30 per cent or so of patients with epilepsy who remain drug resistant.
“In cases of pharmacoresistant epilepsy (PRE) that are severe, you would consider surgery – removal of part of the brain that gives rise to the seizures: the epileptogenic zone.
“A patient will have electrodes implanted into different areas of the brain that have been determined through clinical assessment, imaging et cetera as probably being involved in the genesis of the seizures.
“They will be involved in constant electrophysiological monitoring for about two weeks with the aim of localising the epileptogenic zone.
“Through this, a decision can be taken on whether it can be removed by resection or ablation. In about 30 per cent of cases, this zone lies in an area of high functionality in the brain and it cannot be removed, or it’s inaccessible, or there is not one but multiple epileptogenic zones and you don’t know the relationship between them.
“So there are cases where surgery cannot be performed. In these cases, we believe you can implant a device for localised drug delivery past the blood-brain barrier.
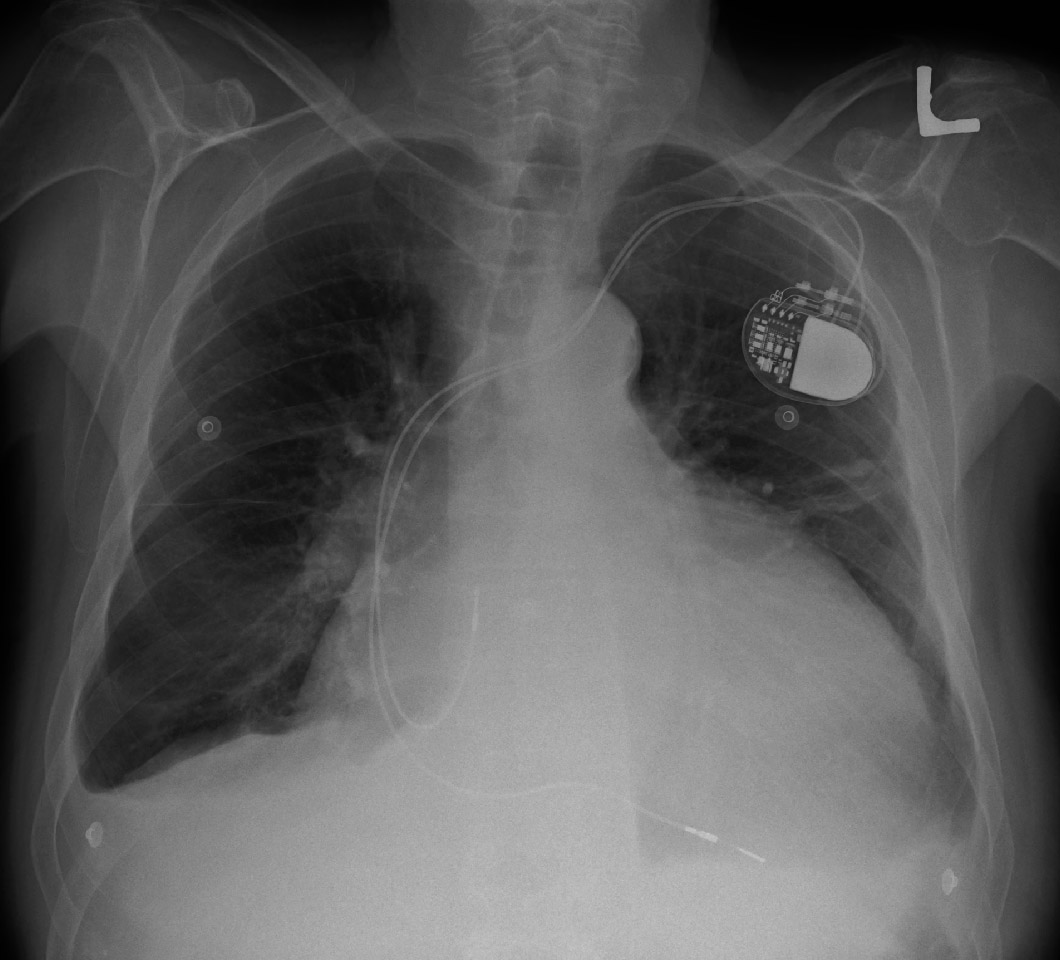
Pacemakers are the most common implantable device today
“Our recent work focuses on this: trying not only to develop the devices that read the brain and detect the origin of the seizures but devices that can deliver drugs.”
An organic electronic ion micropump for implanting in the brain has been developed by Professor Malliaras and fellow researchers in France and Sweden. If successful, it could enable doctors to use a wider gamut of drugs that would, if delivered by conventional methods into the body, be toxic to other organs.
The micropump would also enable the use of drugs that would not normally get past the blood-brain barrier to be delivered directly into the brain – and to the specific area required.
“Also, lower doses can be administered – and only when needed by using a closed-loop system that monitors the brain,” adds Professor Malliaras. “There are a lot of advantages.”
The battery-powered micropump – 20 times thinner than a human hair – has no moving parts. Instead, the pumping is achieved by applying an electric field. It has proved successful in the lab, but the pump has yet to be tested in humans.
“There is quite a lot of work that needs to be done and I believe it’s beyond the scope of a single academic group to take it to the clinic,” says Professor Malliaras.
And he reveals: “We will need a bigger consortium and I’m in the process of doing that here in the context of brain tumours.
“Since I arrived in Cambridge, I’ve found a great opportunity for using this device for cases of brain tumours that are inoperable, such as glioblastomas that lie in an area of the brain with high functionality. It would offer localised chemotherapy.
“That is a new area, but we are being opportunistic. We are a group that develops medical technologies and a large part of the group tries to remain agnostic of the final application. We explore those with different collaborations.”
With any such interface, precision measurements of the brain’s electrical activity are crucial – but embedding electrodes into the brain is a challenging task, which carries the risk of striking a blood vessel.
Professor Malliaras and colleagues have developed a sensor of electric potential that can sit over the brain and measure the activity of a single neuron without disturbing its environment.
“Before this device came along, the only way you could measure single neurons was to penetrate the brain and sit very close to them,” he says.
“We developed a device where we optimised both the mechanical and electrical contact with the brain, which means we can now sit at the surface of the brain and have very small electrodes that form very good contact. They have enough spatial resolution to pick up single neuronal signals. This would be used for more accurate mapping. Before you perform any surgery on brain tumours or epileptogenic zones, you need to map the brain to see what functionality lies there.
“With these electrodes, the mapping can be done much more accurately.
“It’s a bit like clingfilm – it’s four microns thick. If you put it between your finger, you can’t feel it.”
In a paper published in August 2016, Professor Malliaras and colleagues unveiled the ‘bioelectronic neural pixel’ – technology combining this clingfilm-like sensor with the organic electronic micropump.
The system was used to measure epileptic activity in a brain slice model, and delivered neurotransmitter drugs to the same sites to control it.
“We were able to detect activity that was abnormal and then turn on the pump and silence it,” explains Professor Malliaras.
“Both the sensor and the actuator, which is the pump, utilise a conducting polymer which is a material capable of transporting both electronic and ionic carriers. As a result, you can have the same material sensing the electric field and pumping the drug.”
Such a system could be used to treat a range of neurological conditions – and the wider potential of brain interfaces and bioelectronics generally is staggering.
Pharmaceutical giant GlaxoSmithKline and Google’s parent company, Alphabet, through its life sciences division, Verily, took a £540million gamble on the field in 2016 when they formed Galvani Bioelectronics – a name inspired by the Italian physician of frog experiment fame.
From its base in Stevenage, Hertfordshire, Galvani aims to pioneer the use of electrical stimulation as a replacement for systemic drug administration.
“They envisage a future where, instead of taking a pill that goes into your stomach and then throughout your body, you implant a stimulator in the peripheral nerve that tickles that nerve and speaks the language of the signals that are sent from the brain to that organ, and tries to get back to normal function,” says Professor Malliaras.
Galvani’s president, University of Cambridge graduate Kristoffer Famm, has likened the impact that bioelectronics could have on healthcare to the way mobile phones have changed our lives. Altering the signals to organs like the liver, pancreas, kidneys or spleen can alter their behaviour – changing the amount of hormones produced, for example.
Professor Malliaras says: “There are sensors that can sense an electric field but also sensors that sense biomolecular signals, such as metabolic activity. Those are difficult to make and make stable in the body but are much more useful.
“What people are trying to do today is learn the neural code, the signals that the brain uses to communicate with organs using the peripheral nervous system.
“The hope is once you learn that code, you can talk to organs using that language, understand the state of health and whisper them back into normal function when they are off. This is the field of bioelectronic medicine or electroceuticals that Galvani Bioelectronics, along with other companies, is trying to address.”
He adds: “People who study the brain are roughly divided into two camps – the electrophysiologists who look at electrical activity and the people who look at metabolic activity – the imaging people who use MRIs and big machines.
“If you were to have a biochemical sensor that can record metabolic activity at a local level and you could correlate that with electrophysiology, then you bring these two schools of thought together. That is a very high value proposition, I think.”
There is also much work going on in the field to help people with paralysis, either through rebuilding connections in the spinal cord, or bypassing it and stimulating muscles directly using signals picked up from the brain.
“There isn’t anything that works today but there are a lot of people working on it,” says Professor Malliaras.
Although not widely shown on TV, the first kick of the World Cup in Brazil in 2014 was taken by a quadriplegic using a large exoskeleton controlled by his brain.
“With the first pacemaker, the patient wheeled a cart with all the batteries and electronics – that was in 1956-57 before the first fully implanted pacemaker. This is where we are today with exoskeletons,” says Professor Malliaras. “But the pacemaker is a very simple device compared to an exoskeleton driven by brain waves.”
So where could all this go?
“It’s very difficult to predict the pace of the technology,” he says. “If I was able to, I’d probably be retired, sitting under a coconut tree, drinking margaritas…
“But I think there will be better in vitro tools very soon. There are companies working on that, using conducting polymer-like materials to have better interfaces with biology in an in vitro setting for drug discovery, toxicology studies and applications of that type.
“In vivo it’s a much more challenging topic. There is a very large barrier to producing devices with new materials or new fabrication technologies for use in the human body. It’s a liability issue. There is reticence from the chemical industry, for example, to supply material to the implant manufacturer because they are afraid that if the material fails in the human body they will get sued.
“In order for a new technology to make it, there has to be compelling advantages. I think in the case of organic material, there are, so I’m very optimistic about the future.”
Written by Paul Brackley for The Cambridge Independent

