The Institute of Physics and Engineering in Medicine President’s Prize for best oral presentation at the 2017 Medical Physics and Engineering Conference, has been awarded jointly to alumna Cara Cooper and to Matt Smith, a collaborator with Professor Michael Sutcliffe's Biomechanics group.
Great to see these two areas of research on hearing brought together in this joint prize
Professor Michael Sutcliffe
Cara is on a sabbatical from PA Consulting and working in the Clinical Engineering Innovation Group at Addenbrookes Hospital. She is working with Professor John Clarkson's group on healthcare design.

Her prizewinning presentation was on her paper Hear Glue Ear: Horizontal Innovation to provide hearing for children with Glue Ear. Cara, a Medical Device Engineer, is the lead on the Hear Glue Ear project, where she is responsible for the product development, risk management and technical file compilation to the medical devices regulation.
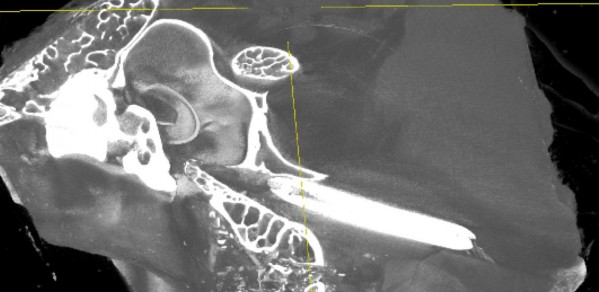
 Matt, an alumnus of the University of Cambridge School of Clinical Medicine, is a Specialist Registrar in Ear Nose and Throat surgery and a Clinical Research Associate, his prizewinning presentation was on his paper: Biomechanical Analysis of Balloon Eustachian Tuboplasty. Matt is undertaking a PhD looking at Eustachian tube dysfunction and possible treatments for it. He is a collaborator with the Biomechanics group in the Department of Engineering, working with Professor Michael Sutcliffe and MEng students Daisy Prior and Anna Weir, with funding from an Engineering for Clinical Practice grant. His current research relates to tests of Eustachian tube function, clinical trials of balloon Eustachian tuboplasty and investigation of the underlying mechanism of Eustachian tube dilatation.
Matt, an alumnus of the University of Cambridge School of Clinical Medicine, is a Specialist Registrar in Ear Nose and Throat surgery and a Clinical Research Associate, his prizewinning presentation was on his paper: Biomechanical Analysis of Balloon Eustachian Tuboplasty. Matt is undertaking a PhD looking at Eustachian tube dysfunction and possible treatments for it. He is a collaborator with the Biomechanics group in the Department of Engineering, working with Professor Michael Sutcliffe and MEng students Daisy Prior and Anna Weir, with funding from an Engineering for Clinical Practice grant. His current research relates to tests of Eustachian tube function, clinical trials of balloon Eustachian tuboplasty and investigation of the underlying mechanism of Eustachian tube dilatation.
By the age of 10 years, 80% of children will have had at least one episode of Otitis Media with Effusion (Glue Ear). Glue ear is a condition in which the middle ear becomes filled with fluid, preventing the ossicles from amplifying sound for the inner ear. The condition is the most common cause of hearing loss and is known to cause fluctuating mild to moderate hearing loss. However, due to spontaneous resolution in 95% of cases, treatments are only offered after extended periods of “watchful waiting” after diagnosis is confirmed through an audiology test. During this time, which can last up to 18 months, hearing aid is rarely provided to the child and this in combination with the condition can result in speech and language problems. Cara and her team aim to transfer consumer bone conduction technology into a medical product which can provide hearing to the child at a low cost. Bone conduction technology by-passes the middle ear and provides sound to the cochlear directly, improving hearing for those with a conductive hearing loss, such as in Glue Ear. This project is delivering a number of complete products which can be used in clinical evaluation as well as developing a technical file sufficient for regulatory approval.
The Eustachian tube is a narrow structure running between the air-filled middle ear space and the back of the nose. It is designed to allow ventilation of the middle ear, but in around 5% of the adult population, the tube fails to open adequately, causing many different types of ear disease. In children, Eustachian tube dysfunction is even more common, often causing glue ear and hearing loss. Until recently, medical staff concentrated on treating the consequences of the disease in the ear rather than the underlying defect with the Eustachian tube itself. Balloon Eustachian Tuboplasty (BET) is a new minimally-invasive technique using a narrow balloon to stretch the Eustachian tube and has recently been used in patients. It appears to be effective at treating conditions caused by poor tube opening. There is much that needs to be understood about how the technique works. In a collaboration between Professor Michael Sutcliffe, Mr James Tysome and Dr Matt Smith they study the biomechanics of balloon inflation within human Eustachian tube tissue. In parallel, physical and 3D computer-based models are created to add to clinical observations and provide methods of testing innovative adaptations to the procedure, and new equipment modifications.
Both Cara and Matt work at the Cambridge University Hospitals NHS Foundation Trust.

